Long Covid: Everything you need to know
What is long Covid?
Definition
Since the beginning of the Covid-19 pandemic, 3 acute forms of the illness have been detected:
- a mild form: it lasts around 14 days between the appearance of symptoms (fever, dry cough, headaches, loss of taste and smell...) and recovery;
- a severe form: initial symptoms are identified in those with the mild form yet more or less severe complications appear (difficulty breathing due to pneumonia and lack of oxygen, inflammatory syndrome, cardiac rhythm problems, formation of blood clots...) that require hospitalisation and sometimes a stay in intensive care;
- an asymptomatic form (40 to 45% of cases): the patient doesn't feel any symptoms but is still contagious.
>>For more information about Covid-19, you can read our article "Is Covid-19 a respiratory illness?"<<
However, after the first wave of Covid-19 cases in Europe, a new form of the disease appeared: this is « long » Covid, also called « persistent » Covid.
Long Covid affects patients who are experiencing persistant symptoms or a resurgence of symptoms, several weeks even several months after the initial disease. These symptoms may appear very debilitating after an obvious recovery.
SARS-CoV-2 is not the first virus to produce long term damage. Viral diseases other viruses such as Ebola, mononucleosis or SARS (Severe Acute Respiratory Syndrome) cause more or less long term problems.
We can also take note of the Chikungunya virus. According to the Pasteur Institute, joint damage caused by the virus may last several months even several years after the primary infection. A South African retrospective study shows that it affects 10% of patients from 3 to 5 years after an acute infection of the Chikungunya virus. In addition, the older age of the patient would be a factor long term damage.
It is important to know the difference between stages of Covid (anatomical lesions and ongoing pathophysiological issues) and problems which develop post-infection from Covid-19.
After much controversy around long Covid (real existence, psychological problems...), this disease is finally recognised by the WHO in its own right since the end of August 2020.
Is long Covid common?
The exact prevalence of long Covid is still not known, but it seems that around 10% of patients continue to have symptoms 3 weeks after the start of the illness.
Long covid affects patients who are suffering from a serious form of the disease, but also patients who have had moderate symptoms.
Furthermore, if long Covid only affects a minority of patients, the considerable number of people who have contracted the disease around the world could cause a real public health problem. However, it is still necessary to collect samples to better understand the potential long-term after effects of COVID-19.
According to the PERSICOR study published in the "Journal of Infection" review, conducted during the « post Covid » consultations from Hotel Dieu in Paris, patients affected by long Covid do not have the biological profile we may expect: they are relatively young, aged between 30 and 60 years, with an average age of 45 years. 79% corresponded to women and half of them played a sport regularly. We can also note that around half of people affected were presenting with an allergic disposition, and 13% had a history of personal or family auto-immune disease.
A national cohort, entitled "Cocolate" was notably put in place by the medical centre in Tourcoing. It includes more than 1000 patients presenting with long Covid and would therefore allow the causes of ongoing symptoms to be identified, to describe the clinical aspects of these symptoms in a precise way and observe their development over time.
Symptoms and complications of long Covid
During the persistence or relapse phase, symptoms may differ from those intitially noticed during first contact with the virus.
These symptoms can be very diverse, as is shown by the fifty or so symptoms below.
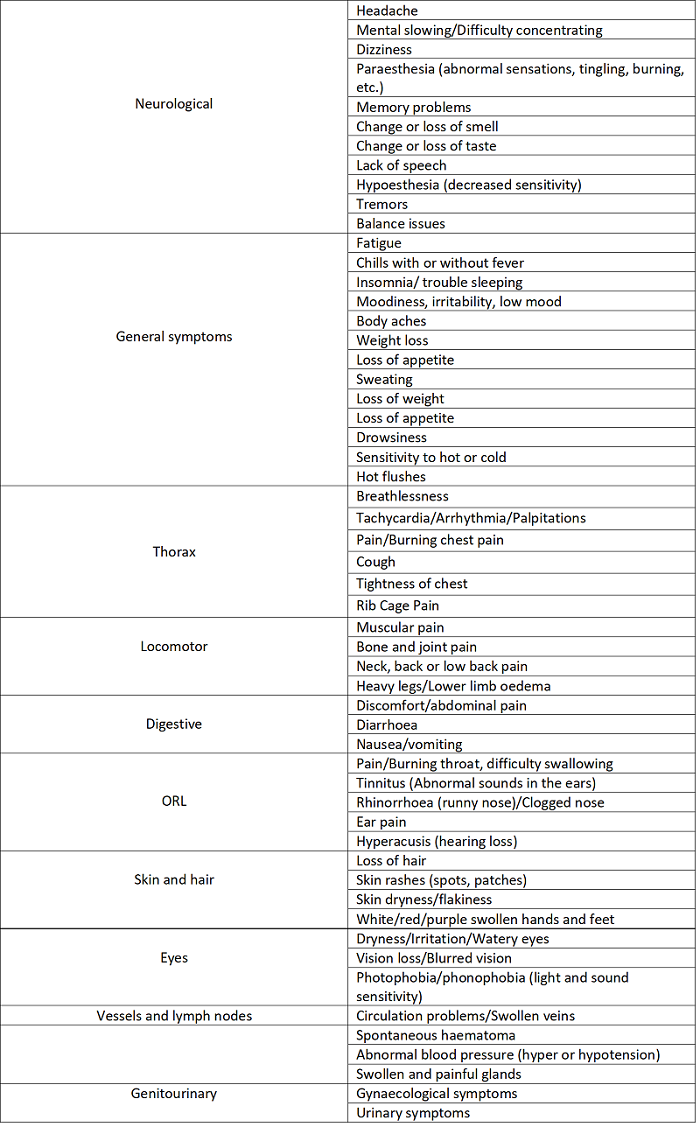
Source: Centers for Disease Control and Protection
The most common symptom mentioned is fatigue, often extreme (asthenia). It is often exacerbated during a little exertion (physical or intellectual) and may force the patient to stop working again, resuming after the illness.
Among the other symptoms often mentioned, it includes breathlessness (dyspnea), a persistant cough, joint and muscle pain, hearing and vision problems, headaches, loss of smell (anosmia) and loss of taste (analgesia), accelerating hair loss (alopecia), as well as lesions in the heart, lungs, kidneys and intestines.
Mental health problems have also been reported, particularly depression and anxiety but also problems with memory and concentration.
These symptoms are fluctuating (alternating between symptomatic periods and periods of remission) and are of varying frequency and durability according to the patients (they can present themselves every week, indeed everyday).
With time, it would appear these phases are less and less important and more and more spaced apart.
Causes and risk factors of long Covid
The causes of long Covid are still not well known, but various hypotheses may be issued:
In rare cases, the virus could remain in the body of certain patients, by reproducing or not, in various places of the body (in particular the nasopharynx and digestive tract).
- a possible reinfection, but rare, by SARS-CoV-2.
- an immune dysfunction (excessive and inappropriate immune response), in people with a particular genetic background, which may cause rheumatism or post-infectious pericarditis.
- chronic fatigue syndrome, also called "myalgic encephalomyelitis", which may occur after an infectious episode
- post-traumatic stress, that may induce somatoform disorders, characterised by symptoms which cannot be explained at the pathophysiological level.
Furthermore, research carried out in men has suggested that SARS-CoV-2 relates to the ACE2 protein (angiotensin-converting enzyme 2) to infect humans and may circulate in the bloodstream to reach several organs.
Researchers at UCLA (University of California in Los Angeles) have also discovered, in genetically engineered mouse models to have the human version of ACE2, that the SARS-CoV-2 virus may stop the production of energy in cells within the heart, kidneys, the spleen and other organs.
Therefore, in addition to temporarily modifying the genes in certain cells, the virus brings epigenetic changes (chemical changes in the structure of the DNA) which causes lasting effects. That may explain why, in certain people affected by COVID-19, the symptoms last over the course of weeks or months after their body has gotten rid of the virus.
A study by King's College London carried out in October 2020 highlighted different possible risk factors of long Covid:
- age (relatively young patients)
- sex (women are more susceptible to developing long Covid)
- overweight (BMI >25 kg/m²)
- asthma
- the presence of more than 5 symptoms during the first week of infection with COVID-19 (for example: cough, fatigue, headache, diarrhoea, loss of smell).
Diagnosis of long Covid
Certain medical exams may be recommended during the persistence of symptoms after an infection of SARS-CoV-2:
- a thoracic angioscanner: to eliminate pulmonary embolism, and identify potential pulmonary lesions;
- an echocardiogram: to identify inflammation of the cardiac muscle (myocarditis) or the membrane that surrounds it (pericarditis);
- an assessment of inflammation;
- an assessment of auto-immunity: protein electrophoresis, autoantibody tests;
- a thyroid assessment
- a serological test (presence of COVID-19 antibodies in the blood or even a PCR analysis (that may indicate the persistence of the virus in the nasopharynx, sometimes more than 6 months after the initial episode).
It is important to note that the Covid test (RT-PCR or serological) can turn out negative in patients affected: a positive test therefore is not a prerequisite for the diagnosis of long Covid.
An electrolyte panel may also be carried out to identify the level of ions in the blood (sodium, chloride, potassium), but also the determination of vitamins and minerals in the blood (vitamin B1, B6, B9, B12, D, copper, zinc, magnesium, calcium, iron).
Long Covid treatments
Even though there are encouraging indications in which certain antivirals or immunosuppressant medications are useful in treating patients in the acute stage of COVID-19, there is no proof that they are useful in the treatment of long Covid syndromes.
Currently, the only indication to use prescription or non-prescription drugs is for the relief of symptoms such as pain and headaches (such as paracetamol).
In addition, the National Academy of Medicine recommends vitamin D supplementation, particularly in patients affected by COVID-19 (to obtain an optimal level around 60ng/mL).
With or without a diagnosis of long Covid, it is required to consider each symptom in order to eliminate potential serious diseases (for example, aspirin has been proven for patients presenting with pericarditis) and to carry out the necessary tests. In particular, various hospitals have opened services to manage long Covid (as is the case for the Hôtel-Dieu hospital in Paris, CHU in Rennes or even CH in Tourcoing).
When a patient presents with hyperventilation syndrome, respiratory and exercise rehabilitation proves useful. It consists of exercise retraining through ventilation and muscular exercises (ergonomic bicycle, treadmill, or rowing machine) and respiratory physiotherapy which allows for bronchial drainage. It can take place in a hospital setting, in specialised centres or at home.
In addition, non-medical treatments, such as physical exercise adapted to the physiology and guided by a health professional, yoga, meditation, hypnosis, acupuncture, but also behavioural and cognitive therapies, can prove useful in managing long Covid.
Finally, it is important to rest and hydrate regularly.
A psychological follow-up may also be useful, particularly in patients affected by anxiety.
Living with long Covid
Some basic tips can help manage your symptoms and improve your everyday life when someone is affected by long Covid:
Managing fatigue and breathlessness
- Adjust your pace of life: plan what you will be doing and don't get too tired.
- Try to divide tasks which seem difficult into several stages and alternate activities from the least difficult to the most difficult.
- Consider the best part of the day to do activities based on your energy level.
- Frequent short breaks are better than some longer breaks: it is important to rest before getting exhausted.
- Don't stop doing things that waste your energy: if you stop using your muscles, they weaken, which can make them more tired when you try to use them
- Try to increase the amount of exercises gradually: take short walks or do simple strength training exercises (such as those set out by the NHS post Covid-19 physiotherapy rehabilitation advice and exercise programme) and increase the length and intensity on an ongoing basis.
Boost your mood and remain in good mental health
- Be indulgent with yourself during your recovery: be prepared for when days are more difficult than others.
- Get in contact with other people (while respecting the rules: telephone, social media and forums such as Carenity, long Covid, or wearing a mask to protect those around you) can help you to feel happier: family, friends, other people suffering from long Covid...
- A patient association supporting your recovery after Covid-19 has also been created to "Bring together and provide information about the long Covid illness in collaboration with researchers and doctors, and to provide support for patients".
- Having a daily routine can help boost your mood and your sense of stability.
- Keep active, continuing to move helps to release endorphins and improve your mood.
Advice for memory and concentration problems
- Take notes to help remember things (during meeting at work or medical appointment for example).
- Try to lower distractions.
- Establish a clear plan to discuss any issues or new or complicated situations. Break it down into steps as you go along.
Relieve joint and muscular pain
- Perform flexibility exercises (such as stretches, yoga, tai-chi), as well as strength exercises (like climbing stairs, lifting appropriate weights, and working with rubber resistance bands). Sometimes it is necessary to consult your doctor before starting an exercise programme for the first time.
It is important to inform your GP about the appearance of health problems after a COVID-19 infection, particularly when they worsen, or new symptoms start to appear. In fact, it is important to note that COVID can also affect pre-existing medical conditions, such as diabetes, where the control of normal blood glucose levels can be affected.
Conclusion
Until now, efforts have mainly been focussed on the fight against the virus and lowering cases of deaths during the pandemic. Nevertheless, today we see the emergence of long-term after effects of COVID-19 infection which needs support.
Faced with these clinical puzzles and a virus in which people have only heard of it being spoken about for a few months, several questions remain unanswered: why do certain people suffer from long Covid? How long does the illness last? And will all patients enjoy a complete recovery? Finally, it is about establishing whether these symptoms are really associated with COVID-19, and if yes, through what mechanisms?
https://www.blf.org.uk/support-for-you/long-covid/what-is-long-covid
https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
https://www.bbc.co.uk/news/health-54296223
https://www.kcl.ac.uk/news/study-identifies-those-most-risk-long-covid
https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html
https://www.youtube.com/watch?v=yb3LAc-GcSU
https://www.scientificamerican.com/article/the-problem-of-long-haul-covid/
Published 9 Jul 2021



