World Glaucoma Day: Let’s take a look at glaucoma
Published 12 Mar 2021 • By Clémence Arnaud
In honour of World Glaucoma Day, let's take a closer look at this serious eye condition. Glaucoma is the second leading cause of blindness in the world, which makes this condition a priority for research.
What is glaucoma? What are the symptoms of this eye condition? How is it diagnosed and what treatments exist for it?
We tell you everything in our article!

Glaucoma: definition
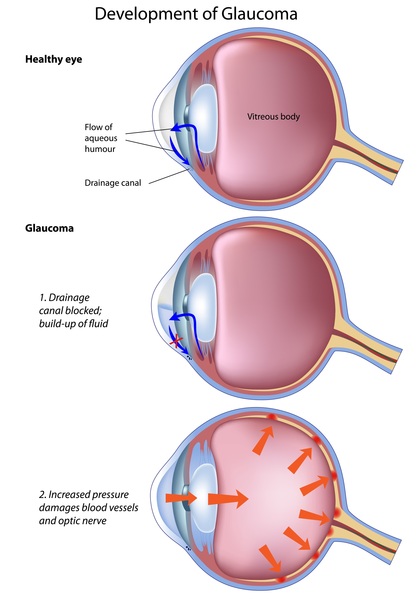
Most cases of glaucoma are caused by an abnormal build-up of pressure in the eye. The optic nerve that transmits information to the brain becomes damaged and no longer performs its role, which can cause the affected eye to go blind. Most of the time, this pressure is due to an accumulation of a fluid (aqueous humour) that flows throughout the eye. This fluid helps to hydrate the eye, eliminate waste products and regulate intraocular pressure by normally draining out from the drainage canal where the iris and cornea meet. But, when there is too much fluid or the drainage system doesn't function, the fluid cannot be evacuated at its normal rate and eye pressure increases.
Glaucoma can be acute with a sudden and sharp increase in internal pressure, but it can also be chronic when the pressure increases slowly and progressively.
Acute glaucoma is also called angle closure glaucoma and is considered a medical emergency. Chronic glaucoma is also referred to as open-angle glaucoma and is the most commonly occurring type, accounting for 80-90% of glaucoma cases.
Source: NIH U.S. Library of Medicine, Medline Plus
Credit: Alila Medical Media/Shutterstock.com
This condition can occur at any age, but its frequency increases with age. In fact, it affects 1 in 10 people over the age of 70. It is important to recognise the hereditary nature of this disease and to introduce screening from the age of 40 onwards for people with a family history of glaucoma. Approximately 30% of glaucoma cases are hereditary in origin.
Glaucoma symptoms
Angle closure glaucoma
This type of glaucoma usually only affects one eye and develops quickly and suddenly. It commonly occurs when the eyes dilate (when the pupils enlarge) too much or too quickly, such as when you enter a dark room or have your eyes dilated by an eye doctor. Symptoms may include:
- Severe eye pain,
- Appearance of rainbow-coloured halos around bright lights,
- Marked visual impairment, such as hazy or blurred vision,
- Redness in the affected eye
This is considered a medical emergency. Older people and those who are farsighted are at greater risk of developing angle closure glaucoma.
Open-angle or chronic glaucoma
This type of glaucoma affects both eyes, often unevenly: one eye is less affected than the other and compensates for the loss of vision. This phenomenon can delay diagnosis. Most people with this type of glaucoma feel normal and do not notice any symptoms or change in vision until the disease is usually quite advanced. Rarely, the person may experience dull pain (such as pressure in the eyes), watery eyes and headaches.
Other symptoms may occur after several years, such as visual impairment, which is a sign of advanced glaucoma. This can include tunnel vision (loss of peripheral vision despite normal central vision).
Diagnosing glaucoma
The diagnosis of glaucoma is made by an ophthalmologist and may take several years.
The intraocular pressure (IOP) must be assessed with a tonometer or a non-contact tonometer (air-puff test). The thickness of the cornea must be also assessed (pachymetry), as it strongly influences IOP.
Ophthalmoscopy (also called funduscopic examination) is used to observe the retina and in the case of glaucoma it is performed to estimate the condition of the optic nerve and nerve fibres. It makes it possible to see the progression of the disease.
Gonioscopy is also performed during the eye exam to examine the eye's internal drainage system, called the anterior chamber angle. This test allows the ophthalmologist to measure the angle between the iris and the cornea - an abnormally narrow angle is associated with an increased risk of acute glaucoma.
Finally, a visual field test can detect dysfunction in central and peripheral vision, which can be a sign of glaucoma.
Monitoring glaucoma
Regular check-ups and monitoring are very important in glaucoma. A full ophthalmic check-up should be performed by an ophthalmologist at least once every two years. The ophthalmologist first needs to make sure that the patient is following treatment properly. It is also important to perform the necessary tests to see how the disease is progressing.
Prevention is important, especially for people with risk factors for glaucoma: those with a family history of glaucoma, those who are extremely near- or farsighted, people over 60, etc. Almost 500,000 people are living with glaucoma in the UK, many of which are living undiagnosed.
Treatments
Eye drops
In the case of chronic glaucoma, eye drops will be prescribed to maintain the intraocular pressure below a certain level to stop the progression of the disease. Proper adherence to treatment is essential to avoid losing sight. It is very important to know that the treatments will not any lost vision, but will limit the progression of the glaucoma and thus preserve the patient's sight.
- Beta-blockers: The most commonly prescribed eye drops are topical beta blocker eye drops which decrease the production of aqueous humour to lower intraocular pressure. However, these drops are contraindicated in some conditions, such as asthma, COPD, heart failure, etc.
- Prostaglandins: Prostaglandin analogue drops increase the drainage of aqueous humour from the eye and are frequently prescribed for glaucoma. A number of side effects have been observed with these drops, most notably change in eye colour, eye redness, and darkening and/or lengthening of the eyelashes.
- Carbonic anhydrase inhibitors: These drops also reduce the production of aqueous humour.
- Alpha-adrenergic agonists: These drops both reduce the production of aqueous humour and increase fluid drainage in the eye.
Combination eye drops also exist, which allow for more than one medication to be used (which is necessary in some cases), but limits the number of necessary applications. These can be prescribed when treatment with a single type of drop has failed, or in case of possible allergic reactions.
Other eye drops are prescribed much less frequently and are designed to alter the diameter of the pupil according to the patient's type of glaucoma: miotics constrict the pupil and mydriatics dilate it.
If eye drops do not improve intraocular pressure, the doctor may suggest laser treatment or even surgery.
Laser treatment
Laser treatment permits medical procedures to be performed on the without having to open it. In the case of glaucoma, it entails aiming a high-energy beam of light at the front segment of the eye to stop the build-up of fluid. The procedure lasts only a few minutes and requires only a local anaesthetic eye drops. After treatment ant-inflammatory drops are prescribed to encourage healing.
Surgery
Surgery is the last-resort treatment for patients suffering from glaucoma. It is performed only when drug treatments or laser have not been efficient enough to control the glaucoma or if eye drops are not tolerated well.
The most common type of surgery for glaucoma is trabeculectomy, in which part of the eye-drainage tubes are removed to facilitate fluid drainage.
Research is ongoing
Research continues in order to develop innovative treatments that are better suited to patients and have new therapeutic goals. This includes the development of eye drops that are better tolerated by patients:
- The CXCR3 receptor for chemokines, the proteins responsible for the inflammation response, seems to be a new area of interest in the development of new glaucoma treatments.
- Rho-kinase inhibitors, or ROCK inhibitors, have also been studied for the treatment of glaucoma and are thought to increase fluid drainage in the eye.
Living with glaucoma
A number of solutions exist to assist patients in adapting their daily lives to the disease, such as low vision rehabilitation with an orthoptist or occupational therapist. Glaucoma is a disease that disrupts patients' lives in many ways. It may be necessary to adapt the patient's professional activity if it puts a lot of strain on the eyes. The patient's physical activity may also need to be modified if the he or she is involved in strenuous or contact activities. It can be more difficult for the patient to be independent when the disease is in an advanced stage and he or she can no longer drive, for example.
Patient associations exist to support patients as they navigate their eye condition, such as the Royal National Institute of Blind People. Some patients may also be eligible for aid.
Was this article helpful to you?
Share your thoughts and questions with the community in the comments below!
Take care!

 Facebook
Facebook Twitter
Twitter



