Medication leaflets made simple: Here’s what you need to know to stay safe
Published 12 Sep 2025 • By Somya Pokharna
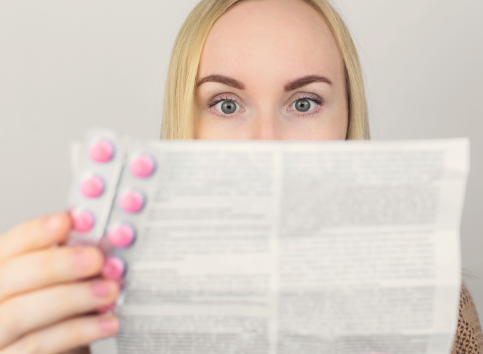
Ever unfolded that tiny, crinkled piece of paper tucked inside your medicine box, only to feel like it was written more to confuse than to help? You’re not alone, and yet that leaflet contains some of the most important information for your health.
This article will help you cut through the jargon and formatting maze to understand what matters most, like what the medicine is, how to take it, what to watch out for, and when to seek help. No pharmacy degree needed, just a little guidance, curiosity, and some easy strategies you can use right now.
What is a medication leaflet, and why is it so confusing?
A medication leaflet, also known as the Patient Information Leaflet, is the official document included with your prescription or over-the-counter medication. It explains the medicine’s purpose, how to use it safely, and lists precautions, possible side effects, and storage recommendations. Although it might feel like dense legalese, this is often because it's designed to meet regulatory standards, so clarity sometimes takes a backseat to compliance.
To make matters worse, these leaflets are typically packed with technical terms, tiny font, and paragraphs that feel never-ending. Research shows that a large proportion of adults struggle with health literacy, meaning even familiar-looking information can be difficult to follow. No wonder they can be overwhelming.
How should you read your medication leaflet?
Start with what matters most
Focus your attention on these key parts first, they tell you everything you need to take your medicine safely:
- What the medicine is and what it's for
- How to take it: dose, timing, whether or not to take with food
- Warnings and precautions: chronic conditions, interactions, lifestyle considerations
- Possible side effects: what you might expect, how often, and how serious
- When to stop and seek help: red flags that warrant immediate contact with healthcare services
You can skim or ignore the manufacturing details, like batch numbers or legal disclaimers, unless something specifically concerns you.
Look for plain language alternatives
If any terms strike you as complicated or unfamiliar, it’s completely normal and fixable. Use trusted online resources, such as the NHS Medicines A–Z, to look up medical jargon in more everyday language. Some apps (like MediSafe or Drugs.com) offer simpler explanations and helpful summaries.
If your leaflet feels especially daunting, see if there’s a version created for easier reading, such as easy-read guides or summaries that aim for clarity.
Use the teach-back method
After reading, explain what you just learned to someone you trust, or simply say it out loud as if you're teaching yourself. This method helps reinforce understanding and reveals any spots you might have misunderstood. It’s a tip supported by healthcare guidelines to improve patient comprehension.
Talk it over with your pharmacist
Pharmacists are a goldmine of practical information, and they’re required to help you understand your medicine. Don’t be shy. Ask questions like:
“What’s the most important thing I should know about this?”
“What should I do if I accidentally miss a dose?”
“Is there something I need to avoid, like foods, activities, or other medicines?”
A quick chat can turn confusing guidance into clear, actionable steps.
Annotate or simplify for yourself
As you read, highlight or underline the most important points. Rewrite key details in your own words. For example, a one-page summary stuck to your fridge or medicine cabinet can be a lifesaver. Use simple icons or your own shorthand, something you’ll clearly understand in a moment of need.
Why is it so important to carefully read and understand medicine leaflets?
Medication errors aren't just embarrassing; they can be dangerous. Studies show that preventable medication-related harm affects around 3% of patients in healthcare settings worldwide, and a significant portion of these cases are serious or even life-threatening. In fact, medication errors account for a substantial share of all harm caused by preventable medical mistakes.
Being confident in what your medicine does, and how to take it, helps you avoid:
- Taking the wrong dose or taking it at the wrong time
- Dangerous interactions with other medications or common foods
- Confusion about side effects, whether they’re normal or require medical attention
On the flip side, clear understanding promotes adherence, meaning you’re more likely to take your medicine as prescribed, and reduces anxiety. It empowers you to make informed decisions, advocate for your health, and avoid unnecessary complications or hospital visits.
As research into health literacy shows, simplifying language, encouraging questions, using teach-back, and visual aids all measurably improve outcomes, especially for older adults or those managing multiple medications.
Key takeaways
You don’t need a pharmacy degree to make sense of your medication leaflet, just a plan, a few tools, and the confidence to ask for help when you need it. Here's your roadmap:
- Start with the essentials: what it’s for, how to take it, side effects, warnings, and when to seek help.
- Simplify language: use trusted resources or apps to translate medical terms into plain English.
- Teach-back is your friend: repeat the info back in your own words.
- Ask your pharmacist: clarify important details, no question is too small.
- Create your own clarity: annotate or summarize in a way that works for you.
Ultimately, understanding what’s written on that small piece of paper could make a big difference, helping keep you safe, informed, and empowered in your health journey.
Did you find this article helpful?
Give it a “Like” and share your thoughts and questions with the community in the comments below!
Take care!
Sources:
An Introduction to Health Literacy. (2021). Network of the National Library of Medicine.
Avoiding preventable harm. (2024, May 24). Washington State Nurses Association.
Bates, D. W., Levine, D. M., Salmasian, H., Syrowatka, A., Shahian, D. M., Lipsitz, S., ... & Mort, E. (2023). The safety of inpatient health care. New England Journal of Medicine, 388(2), 142-153.
Courtney, B. (2025, March 6). Medication Error Statistics 2024. DosePacker.
Elliott, R. A., Camacho, E., Jankovic, D., Sculpher, M. J., & Faria, R. (2021). Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Quality & Safety, 30(2), 96-105.
Global burden of preventable medication-related harm in health care: a systematic review. (2024). World Health Organization.
Hodkinson, A., Tyler, N., Ashcroft, D. M., Keers, R. N., Khan, K., Phipps, D., ... & Panagioti, M. (2020). Preventable medication harm across health care settings: a systematic review and meta-analysis. BMC medicine, 18(1), 313.
Marvanova, M., Roumie, C. L., Eden, S. K., Cawthon, C., Schnipper, J. L., & Kripalani, S. (2011). Health literacy and medication understanding among hospitalized adults. Journal of hospital medicine, 6(9), 488-493.
Medication Errors. (2019, July 18). Academy of Managed Care Pharmacy.
Patients with low health literacy make more errors interpreting instructions and warnings. (2023, November 30). Institute for Safe Medication Practices.
Rodziewicz, T. L., Houseman, B., Vaqar, S., & Hipskind, J. E. (2024). Medical error reduction and prevention.[Updated 2024 Feb 12]. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
Tool: Teach-Back. (2020). Agency for Healthcare Research and Quality.
Yin, H. S., Parker, R. M., Wolf, M. S., Mendelsohn, A. L., Sanders, L. M., Vivar, K. L., ... & Dreyer, B. P. (2012). Health literacy assessment of labeling of pediatric nonprescription medications: examination of characteristics that may impair parent understanding. Academic pediatrics, 12(4), 288-296.

 Facebook
Facebook Twitter
Twitter


