Rheumatoid arthritis and osteoarthritis: How are they similar and different?
Published 7 Mar 2022 • By Courtney Johnson
There are more than 100 types of arthritis and related joint conditions. Two that you may have heard about the most are rheumatoid arthritis (RA) and osteoarthritis (OA).
What are these two joint diseases? How are they similar? And how are they different?
We explain it all below!

What is arthritis? What are rheumatoid arthritis and osteoarthritis?
Arthritis is a very common, but poorly understood condition. While many of us may refer to “arthritis” meaning one condition, it is in fact not a single disease. Arthritis is an umbrella term for more than 100 different diseases affecting the joints, including rheumatoid arthritis (RA) and osteoarthritis (OA).
Both conditions affect the joints but have different causes and symptoms.
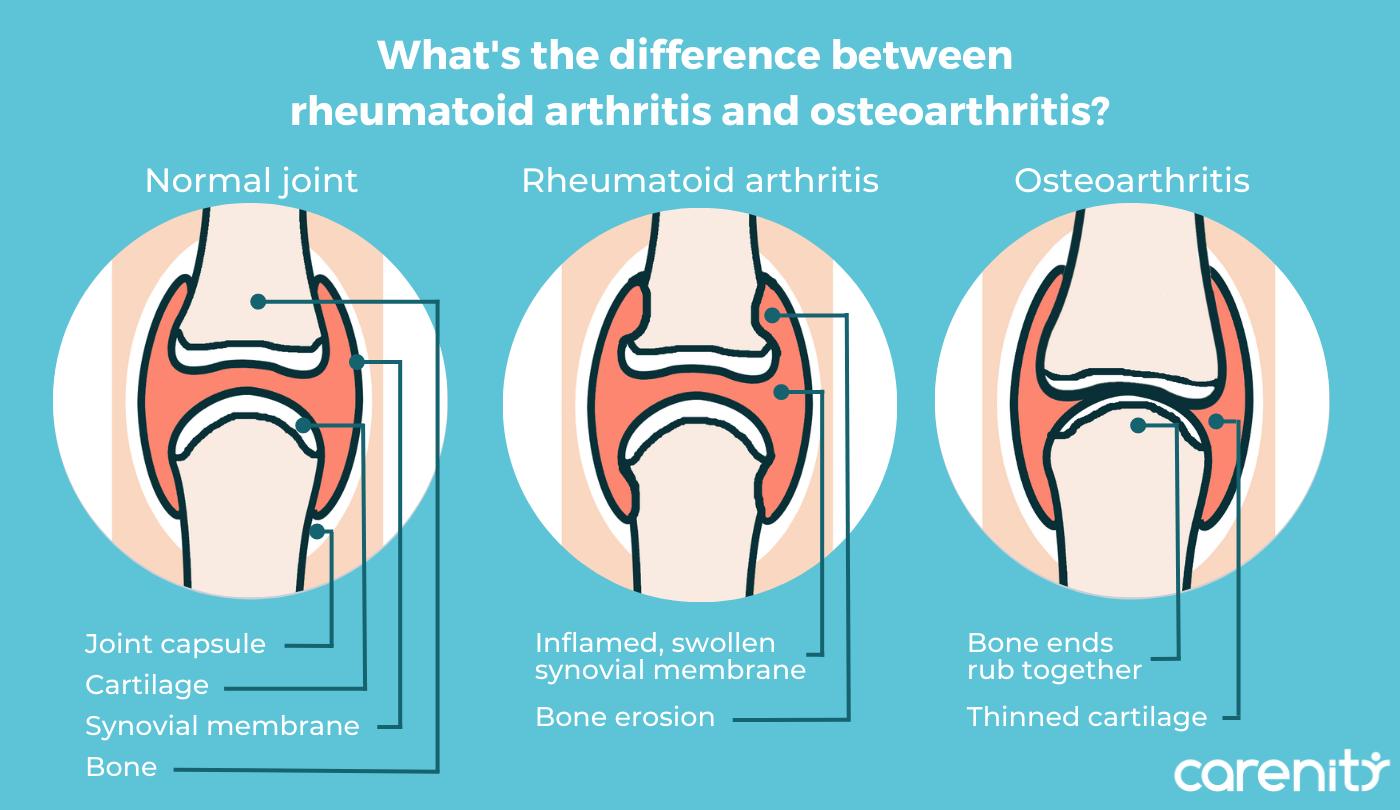
Rheumatoid arthritis is a systemic autoimmune disorder where the immune system overreacts against the body and attacks the lining of the joints, called the synovium. This immune attack causes the synovium to become inflamed, producing fluid which builds up in the joints, causing pain, inflammation, stiffness, and decreased flexibility of the joints.
Osteoarthritis is a degenerative disorder involving the wear and tear of the cartilage, which gradually breaks down and causes bones to rub together. This rubbing between the bones exposes small nerves, causing pain. Though the immune system is not involved in OA, mild inflammation still does occur.
OA is the most common type of arthritis, with more than 8.5 million people in the UK affected, while around 400,000 people are living with RA.
How are rheumatoid arthritis and osteoarthritis similar and different?
Rheumatoid arthritis and osteoarthritis share many of the same core symptoms, which include:
- Joint pain and stiffness
- Restricted mobility in affected joints
- Swelling, which is more severe in RA
- More intense symptoms in the morning
Rheumatoid arthritis characteristics
Rheumatoid arthritis is a systemic condition, which means it can impact the entire body – the lungs, the heart, the skin – and not just the joints. Early symptoms of RA can include:
- Intense fatigue
- Muscle ache
- Low-grade fever, particularly in children
RA typically develops first in the smaller joints, such as the hands and finger joints. With time, RA may progress into the larger joints, like the knees, ankles, or shoulders. Additionally, RA is a symmetrical condition, meaning that symptoms are experienced on both sides of the body simultaneously.
Patients with advanced RA may observe firm lumps or masses under the skin near the joints. These masses are called rheumatoid nodules and can cause tenderness and discomfort.
Osteoarthritis characteristics
Because of its degenerative nature, OA symptoms are limited to the joints, so systemic symptoms are unlikely.
Like RA, osteoarthritis is common in the fingers and hands. It also frequently affects the knees, hips, and spine. OA is a less symmetrical disease. A patient may experience pain in both knees, for example, but one joint or one side may be worse.
Patients may develop masses under the skin near the joints, but these are different than rheumatoid nodules. When they occur in the finger joints closest to the fingertips, they are called Heberden’s nodes, and when they are in the middle joints, they are called Bouchard’s nodes. These bony swellings commonly occur as Heberden's nodes and can cause pain and deformation of the fingers.
People with OA are also more likely to develop bone spurs (osteophytes), which are bony projections that develop where bones meet – in the joints.
Both forms of arthritis occur more commonly in women than in men and are more frequent in older adults, though RA can develop at any age.
RA also has a hereditary factor – a person has a higher chance of developing it if a parent, sibling, or child has it.
The likelihood of developing OA increases if you:
- Are overweight or obese
- Have diabetes
- Have gout
- Have joint deformities
- Have experienced a traumatic joint injury
What are the treatment approaches for rheumatoid arthritis and osteoarthritis?
RA and OA are two chronic illnesses, meaning that they do not go away. There is no cure for either disease, but treatments can help patients to manage symptoms, slow disease progression, and improve quality of life.
In both conditions, the treatment objectives are to:
- Reduce pain
- Improve joint mobility and function
- Limit damage to the joints
Treatment strategy, however, will differ depending on whether the patient has RA or OA.
Common treatment regimens include medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation, ease pain and stiffness, and improve range of motion.
Doctors may also use steroid-based medicines to treat inflammation. These may be injected directly into the joint to treat inflammation quickly and at the source during a flare-up.
For RA, the American College of Rheumatology recommends the use of disease-modifying antirheumatic drugs (DMARDs), in combination with NSAIDs or steroids and biologics. DMARDs are designed to block the inflammatory process by suppressing the immune system, therefore reducing damage to tissues and joints.
For OA, the College recommends topical and oral NSAIDs, steroid injections, in addition to self-management approaches like diet, exercise, and medical devices or aids.
Physical therapy can be beneficial in both RA and OA, as it helps to improve mobility and maintain joint flexibility.
Finally, a number of lifestyle changes are advisable for both conditions. Following a healthy and balanced diet and following a regular, adapted exercise plan can also aid. Maintaining a healthy weight can reduce pressure on the joints and ease symptoms. Stopping smoking and avoiding second-hand smoke are also recommended, especially for RA patients.
Was this article helpful to you?
Give it a like and share your thoughts and questions with the community in the comments below!
Take care!
Sources:
What is RA, National Rheumatoid Arthritis Society
Arthritis, NHS
Rheumatoid Arthritis, American College of Rheumatology
Osteoarthritis, American College of Rheumatology
Rheumatoid Arthritis: Causes, Symptoms, Treatments and More, Arthritis Foundation
What is Arthritis?, Arthritis Foundation
Singh, J.A., Saag, K.G., Bridges, S.L., Jr., Akl, E.A., Bannuru, R.R., Sullivan, M.C., Vaysbrot, E., McNaughton, C., Osani, M., Shmerling, R.H., Curtis, J.R., Furst, D.E., Parks, D., Kavanaugh, A., O'Dell, J., King, C., Leong, A., Matteson, E.L., Schousboe, J.T., Drevlow, B., Ginsberg, S., Grober, J., St.Clair, E.W., Tindall, E., Miller, A.S. and McAlindon, T. (2016), 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis & Rheumatology, 68: 1-26. https://doi.org/10.1002/art.39480
Treatment Guidelines for Osteoarthritis, Arthritis Foundation
How Are Rheumatoid Arthritis and Osteoarthritis Different?, Healthline
Rheumatoid Arthritis vs. Osteoarthritis Joint Pain, Everyday Health
What’s the difference between rheumatoid arthritis and osteoarthritis?, MedicalNewsToday
3 comments

You will also like

In fibromyalgia, cognitive symptoms are worse than in rheumatoid arthritis
28 Jun 2016 • 21 comments

Rheumatoid arthritis: "I never tried to accept the disease but to move forward"
20 Mar 2021 • 5 comments

 Facebook
Facebook Twitter
Twitter
